Have you ever heard of the “obesity paradox?” This refers to a healthcare phenomenon that while high BMI is often cited as a major risk factor for cardiovascular disease, when a cardiac event does occur, these patients manage to have a high survival rate.
Additionally, many patients with high BMI have better surgical outcomes and live longer than men of a “typical” BMI with those same illnesses.

What Does the Medical Field Get Wrong About Fat People?
We are always bombarded by messages from healthcare professionals, family members, and “concern trolls” that our weight is detrimental to our health. The truth is a lot of older research that “supported” that claim is correlational and not causational.
Scholars now believe, based on current research, that the association between weight and health can be explained by factors like body-related stigma, avoidance of healthcare, or poor treatment by healthcare providers.
Where Does the Lack of Knowledge About Plus Size People in Healthcare Come From?
Doctors are taught very little about plus size people in medical school. They are not taught how to talk to fat folks in a meaningful way, they are not taught about fat stigma, or how to check their own biases.
Often, primary care physicians will offer nutrition advice to fat patients completely unprompted. However, during their medical school education, most students spend fewer than 20 hours focused on nutrition. The time that is nutrition-focused does not include meal planning or how to ask patients about their daily eating habits through the use of motivational interviewing.

You may be shocked to learn that fat people cannot donate their bodies to science. Many body donation programs including Mayo Clinic, Yale School of Medicine, and UCLA Health will not accept bodies for post-mortem research over a certain BMI.
This excludes a large part of the US population. How are medical students supposed to learn about fat bodies without being given the opportunity to study them?
Other Examples of Fat-Bias in Medicine
If you’ve ever attempted to look into being a bone marrow donor, you’d notice there is a BMI limit. Medical professionals may have been able to justify this in the past because of where bone marrow is harvested from, making it “more difficult” on someone who has more body fat. However, currently 83% of donations are peripherally collected, making that argument completely fall apart.
Even to receive an organ transplant, you must be under a certain BMI. This leads us to question, “So I am too fat to save a life? And I’m too fat to be saved myself?” Dr. Rebecca Pohl, the director of research and weight stigma initiatives at the Rudd Center for Food Policy & Obesity at Yale University states, “We know that weight stigma is very prevalent in the health care environment, and that plays out in numerous ways. Sometimes it’s very overt and occurs in patient-provider interactions and sometimes it occurs on a much more complex level related to access to treatment, denial of services, and it gets couched in this more complex conversation of medical risk, and justification of all of these different, safety issues. But then, we really have to make sure that that’s legitimate as in some cases there may be legitimate medical risks. But in some cases, there may not.”
Did you know that fat people need longer needles for vaccines? This was something that was discussed when the Covid-19 vaccine became available. A 2022 paper in the Vaccine journal points to existing needle-length guidelines for vaccines and suggests that some people, especially over a certain weight might not be getting properly immunized against Covid-19 because standard needles are unable to penetrate the deltoid muscle.
The Centers for Disease Control and Prevention (CDC) doesn’t offer specific guidance for needle length in Covid-19 vaccines but gives general guidelines for intramuscular shots, saying a one-inch needle is sufficient for adults assigned female at birth and weighing less than 200lbs. This guidance is consistent for HPV, tetanus, flu shots, any vaccine that is administered intramuscularly.
Discussion regarding the effectiveness of emergency contraceptives in folks with a higher BMI is a hot topic that re-surfaces every few months on social media. Dr. Alison Edelman, a professor of obstetrics and gynecology at Oregon Health and Science University states, “When contraception was developed, it was really a one-size-fits-all model, but our population now is very different from the population when the drugs were developed and we are concerned that the most common type of emergency contraception may not work for women with higher BMIs.”
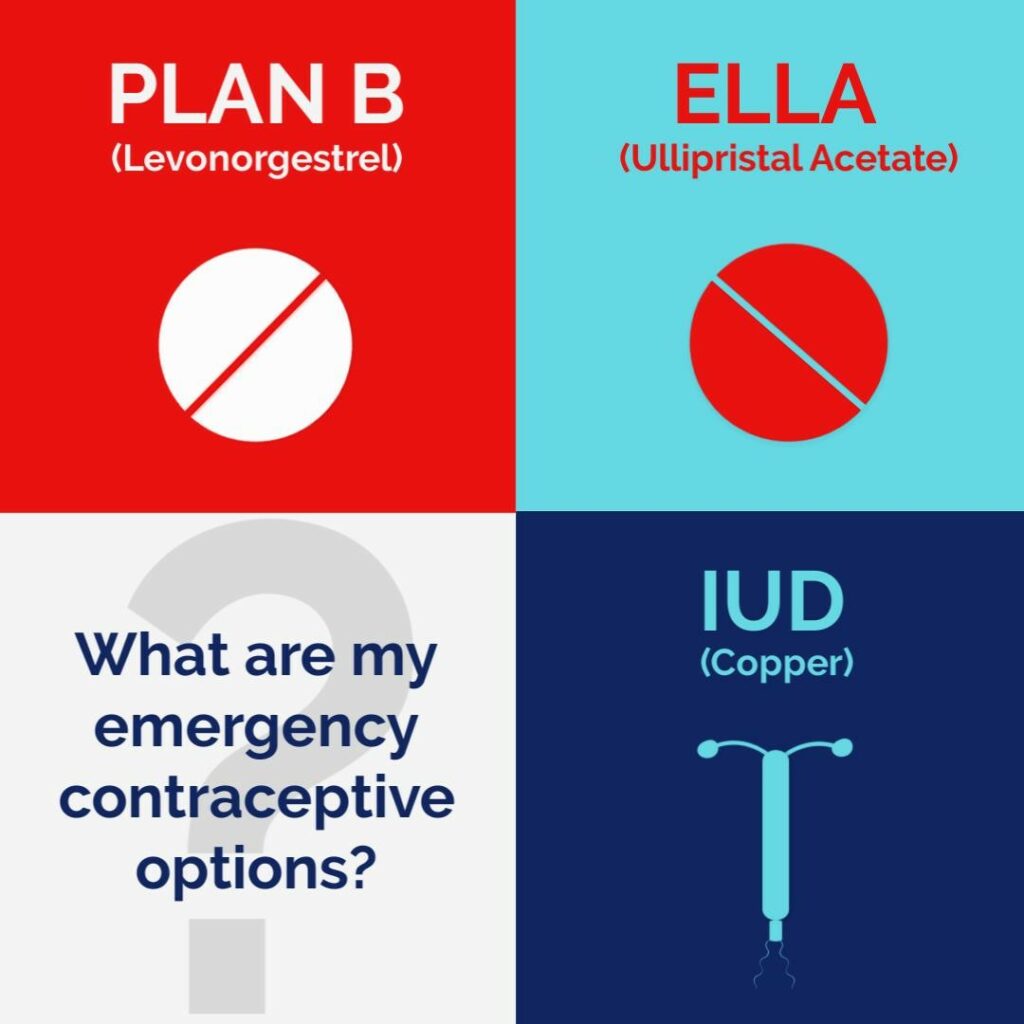
The two emergency contraceptive pills available in the US are Plan B and Ella. There have been studies on both as an attempt to determine is there is a weight-related effectiveness threshold. However, these studies come to different conclusions.
The Food and Drug Administration (FDA) reviewed Plan B and found the data was conflicting and too limited to come to a definitive conclusion whether it was less effective in women who weigh more than 165lbs or have a BMI over 25. A study from Scotland indicated Plan B may be less effective in women over 170lbs.
This leads many doctors to recommend Ella, especially for fat folks. Ella appears to not have as much of a decrease in effectiveness for people with higher BMIs, but it still claims to be the most effective in people under 195lbs.
Is Anyone Actively Looking To Include Fat Folks In Healthcare?
Yes! The All of Us Research Program is seeking to include people who would typically be excluded from medical research. Unlike many research studies that focus on a specific disease or population, this program, through the National Institutes of Health (NIH), is providing a national research resource for thousands of research questions and covering a wide variety of health conditions.
1 million+ diverse participants contribute to electronic health records (EHRs), biospecimens, surveys, and other measures to build a comprehensive set of data that will be open world-wide to researchers.
There has also been an increase in researching weight stigma, how poor evidence-based care impacts the fat community, and the reasons behind fatphobia in medicine.
People like The Fat Doctor (@fatdoctoruk on TikTok) are sharing their first-hand experience and knowledge of the medical industry to spread a weight-inclusive message to their followers.

There are numerous dietitians and nutritionists on social media that work to spread similar messages while working in a field that often does not appear to be size-inclusive, like @yourdietitianbff, @elainaefird, and @findfoodfreedom.
It is our hope that with more size-inclusive advocates and medical researchers that keep their fat-biases in check, one day we will have better access to evidence-based medicine.
One day, we won’t be an afterthought.
One day, we will be actively included in medical research.
One day, we won’t be seen as unworthy.











Bravo Christine.. keep on ranting 👍🏽
Wonderful essay! People come in all shapes and sizes! It’s time that we figured that out!
A wonderful essay!